
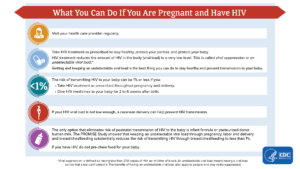
 This is vital to understand for many of these women are of childbearing age. In fact, every year, approximately 5,000 women with HIV give birth in the United States. In addition to primary prevention of HIV infection in people who can become pregnant, the best way to prevent HIV acquisition in infants is to focus on appropriate overall medical care for women, transgender men, and gender-diverse individuals with HIV; this includes comprehensive reproductive health care, family planning and preconception care services, optimization of HIV treatment, and maintenance of care between pregnancies. A critical component of preventing perinatal HIV transmission is ensuring that a pregnant person with HIV receives ART that maximally suppresses viral replication as early as possible during pregnancy or, ideally, before conception. Without treatment, 25 to 30% of babies born to a mother living with HIV will get HIV. However, if mothers are aware of their HIV infection and treated along with their infants, the chances of the infant getting HIV are less than 2%. Because of the advances in HIV research, prevention, and treatment it is possible for people with HIV to give birth to babies who are free of HIV.
This is vital to understand for many of these women are of childbearing age. In fact, every year, approximately 5,000 women with HIV give birth in the United States. In addition to primary prevention of HIV infection in people who can become pregnant, the best way to prevent HIV acquisition in infants is to focus on appropriate overall medical care for women, transgender men, and gender-diverse individuals with HIV; this includes comprehensive reproductive health care, family planning and preconception care services, optimization of HIV treatment, and maintenance of care between pregnancies. A critical component of preventing perinatal HIV transmission is ensuring that a pregnant person with HIV receives ART that maximally suppresses viral replication as early as possible during pregnancy or, ideally, before conception. Without treatment, 25 to 30% of babies born to a mother living with HIV will get HIV. However, if mothers are aware of their HIV infection and treated along with their infants, the chances of the infant getting HIV are less than 2%. Because of the advances in HIV research, prevention, and treatment it is possible for people with HIV to give birth to babies who are free of HIV.
The good news is that the annual number of diagnoses of perinatal HIV in the United States and dependent areas has declined by more than 95% since the early 1990s but it remains vital for each woman to become more aware of prevention strategies – HIV can be passed to a baby during pregnancy, childbirth, and breast feeding; this is called perinatal transmission. So, If you are pregnant or planning to get pregnant, get tested for HIV as soon as possible. If you have HIV, the sooner you start treatment the better—for your health and your baby’s health, and to prevent transmitting HIV to your sex partner. If you don’t have HIV, but your partner does, ask your health care provider about medicine to prevent HIV, called pre-exposure prophylaxis (PrEP). You can also talk to your health care provider about timing sex without a condom to coincide with ovulation to reduce the chances of HIV transmission and increase the likelihood of getting pregnant.

For more information:
-
How likely is mother-to-child transmission of HIV?
https://www.aidsmap.com/about-hiv/how-likely-mother-child-transmission-hiv
-
Having a baby when you are living with HIV
-
https://www.aidsmap.com/about-hiv/having-baby-when-you-are-living-hiv
-
Recommendations for the Use of Antiretroviral Drugs During Pregnancy and Interventions to Reduce Perinatal HIV Transmission in the United States https://clinicalinfo.hiv.gov/en/guidelines/perinatal/introduction
-
HIV and Perinatal Transmission: Preventing Perinatal HIV Transmission
https://www.cdc.gov/hiv/group/pregnant-people/transmission.html
-
Reduce the rate of mother-to-child HIV transmission
https://health.gov/healthypeople/objectives-and-data/browse-objectives/sexually-transmitted-infections/reduce-rate-mother-child-hiv-transmission-hiv-06
-
Preventing Perinatal HIV Transmission
